Pressure ulcers, alternatively referred to as bedsores or pressure injuries, occur when prolonged pressure, friction, or shearing forces lead to localized damage in the skin and underlying tissues. These injuries commonly occur in individuals who are immobile or have limited mobility, such as those confined to bed or a wheelchair. Clinical pressure area assessment is a systematic approach used by healthcare professionals to evaluate and document the risk and presence of pressure ulcers in patients.
1. Purpose:
The primary purpose of clinical pressure area assessment is to identify individuals at risk of developing pressure ulcers and to provide appropriate preventive measures. Additionally, it helps in identifying existing pressure ulcers, determining their severity, and guiding appropriate treatment interventions.
2. Assessment Components:
Clinical pressure area assessment typically involves the following components:
a. Risk Assessment:
– Assessing the patient’s overall health status, mobility, and activity level.
– Identifying specific risk factors such as immobility, malnutrition, moisture, and compromised sensory perception.
– Using standardized tools like the Braden Scale or Norton Scale to quantify the patient’s risk level.
b. Skin Inspection:
– Examining the patient’s skin for any signs of redness, discoloration, blanching, or abnormalities.
– Assessing the integrity of the skin, including areas prone to pressure ulcer development, such as bony prominences (e.g., sacrum, heels, hips, back of head, shoulders, buttocks, elbows, toes, ears, spine and temporal region of the skull).
c. Tissue Assessment:
– Palpating the skin and underlying tissues to assess for temperature, firmness, and the presence of swelling or oedema.
– Documenting any pain or tenderness experienced by the patient.
d. Mobility and Activity Assessment:
– Evaluating the patient’s ability to independently change positions or reposition themselves.
– Assessing the need for assistance or adaptive equipment to optimize mobility and reduce pressure.
3. Documentation:
Accurate and detailed documentation is essential for clinical pressure area assessment. The following information should be recorded:
– Patient demographics and medical history
– Risk assessment score
– Specific sites at risk or existing pressure ulcers
– Description of the skin and tissue condition (e.g., intact, erythema, blisters, necrotic tissue)
– Size, stage, and severity of any identified pressure ulcers
– Pain or discomfort reported by the patient
– Interventions implemented or recommended for prevention or treatment
4. Preventive Interventions:
Based on the assessment findings, healthcare professionals should implement appropriate preventive interventions, including:
– Regular repositioning to reduce pressure and shear forces.
– Use of pressure redistribution surfaces, such as specialized mattresses or cushions.
– Maintaining good hygiene and skin care.
– Adequate nutritional support to promote tissue healing.
– Education and training for patients and caregivers on pressure ulcer prevention.
Clinical pressure area assessment plays a crucial role in identifying individuals at risk of pressure ulcers, facilitating early intervention, and promoting optimal patient care. By implementing preventive measures and timely interventions, healthcare professionals can help minimize the occurrence and severity of pressure ulcers, leading to improved patient outcomes.
Signs of Pressure Ulcer Development:
- Skin Discoloration:
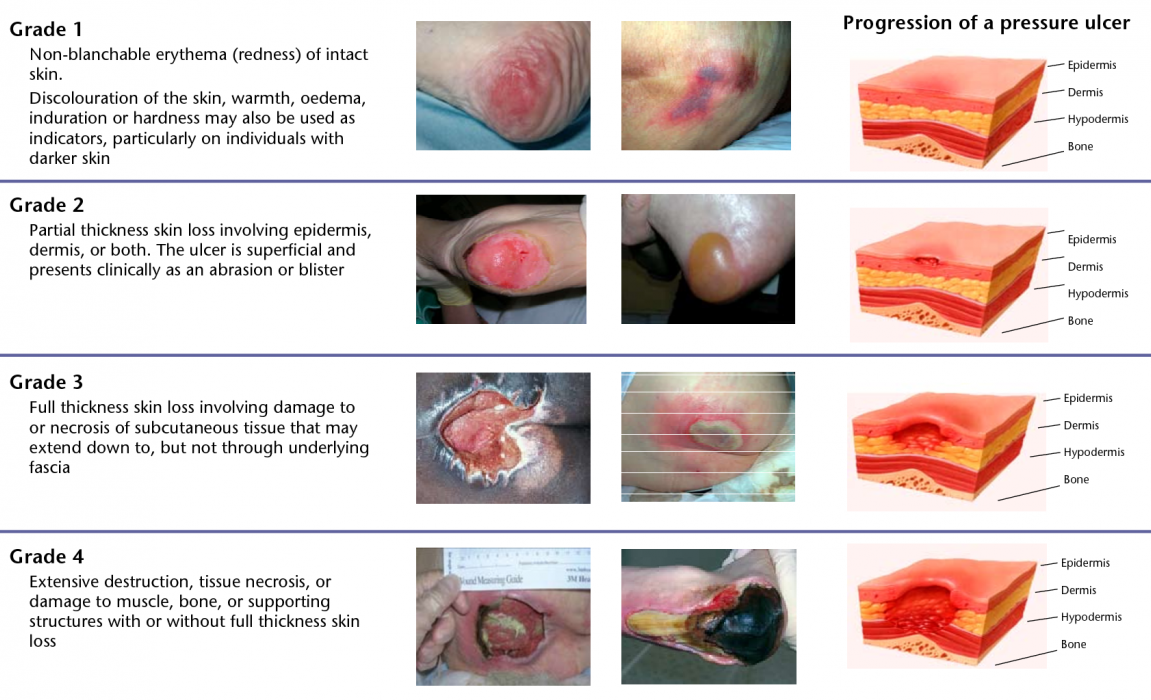
- Redness: Persistent redness in lighter-skinned individuals, or purple or blue hues in darker-skinned individuals, is an early sign of pressure ulcer development.
- SkinTextureChanges:
- Warmth or coolness: The affected area may feel warmer or cooler than the surrounding skin due to altered blood circulation.
- Swelling or oedema: The skin may appear swollen or puffy, indicating fluid accumulation in the tissues.
- Pain or Sensitivity:
- Patients may report localized pain, tenderness, or discomfort in areas subjected to pressure.
- Pain may be present even before visible signs of ulceration.
- Skin Changes:
- Dryness: The skin may become excessively dry, increasing the risk of friction and shear.
- Blister Formation:
- Formation of fluid-filled blisters or vesicles may occur in more severe cases of pressure ulcers.
- Breakdown of Skin:
- Open wounds or ulcers: The skin may break down, forming open wounds that can range in severity from superficial to deep and extending into underlying tissues.
- Underlying Tissue Changes:
- In advanced pressure ulcers, underlying tissues such as muscles, tendons, or bones may become visible.
It’s important to note that pressure ulcers can progress rapidly, especially in individuals with compromised health or limited mobility. Prompt recognition and intervention are crucial to prevent further deterioration and promote healing. Healthcare professionals should regularly assess at-risk individuals and be vigilant for any signs of pressure ulcer development. Like Blisters, Discolouration, Localised heat, Localised Oedema, Localised indurations (abnormal hardening), Purplish or bluish localised areas, Localised coolness if tissue death has occurred
BRADEN SCALE FOR PREDICTING PRESSURE SORE RISK file: