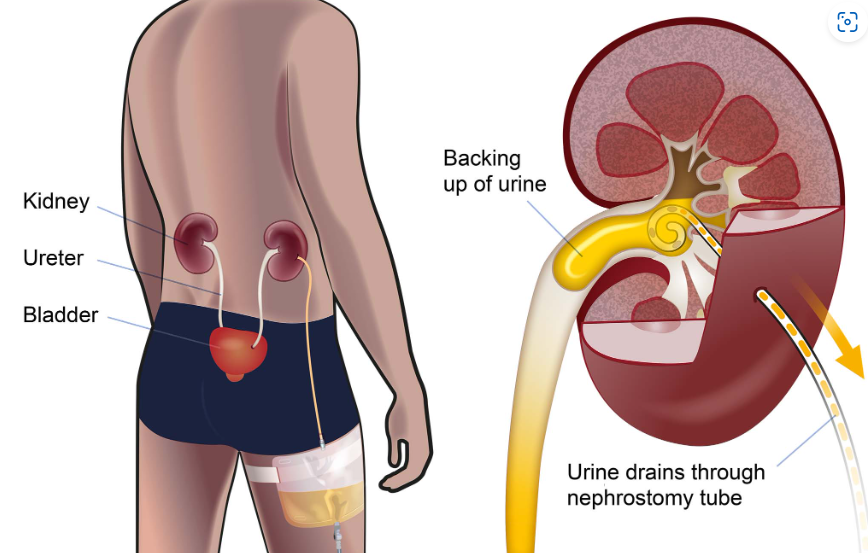

What is a Nephrostomy?
A nephrostomy is a procedure where a catheter (tube) is inserted through the skin into the kidney to drain urine directly from the renal pelvis. It bypasses the ureter, which may be blocked due to:
Kidney stones
Tumours
Infections
Trauma
Congenital abnormalities
The tube exits through the back and connects to an external drainage bag.
2. Comprehensive Nursing Care in the Ward
Initial Post-Procedure Care
Monitor vital signs: Especially in the first 24 hours for signs of bleeding or infection.
Observe the nephrostomy site:
Check for redness, swelling, discharge, or leakage.
Ensure dressing is clean and secure.
Urine output:
Measure and record output hourly initially, then per shift.
Monitor for changes in colour, clarity, or presence of clots.
Ongoing Nursing Care
Site care:
Clean the insertion site daily or as per hospital protocol using aseptic technique.
Change dressing if wet, soiled, or loose.
Drainage bag management:
Keep below the level of the kidney to prevent backflow.
Empty when 2/3 full, using clean technique.
Maintain accurate intake/output charting.
Prevent dislodgment:
Secure the tube with tape or fixation device.
Educate the patient to avoid pulling or tugging.
Infection control:
Watch for fever, chills, increased WBCs.
Report cloudy or foul-smelling urine.
Pain management:
Administer analgesics as prescribed.
Monitor for signs of discomfort, especially during movement or dressing changes.
Patient education:
Explain the purpose and care of the nephrostomy.
Involve them in simple care if appropriate (e.g., emptying the bag).
3. Dietary Management
Hydration: Encourage fluid intake (unless contraindicated) to flush the kidneys.
Low-sodium diet: Reduces kidney strain and manages blood pressure.
Protein moderation (especially in renal impairment): Prevents further kidney burden.
Avoid oxalate-rich foods (if stones are a cause): Spinach, nuts, chocolate.
Monitor electrolytes:
Adjust diet based on lab results (e.g., potassium or phosphate levels).
Consult a renal dietitian for individualized dietary planning.
4. Physiotherapy Management
Mobilization:
Early ambulation if stable to prevent complications like DVT or pneumonia.
Encourage movement while securing nephrostomy tubing to prevent dislodgement.
Breathing exercises:
Especially post-op or if patient is bedridden.
Postural care:
Ensure the patient maintains good posture during bed rest to avoid pressure ulcers.
Pelvic floor or core strengthening (if appropriate):
Improves overall abdominal and back support for long-term nephrostomy patients.
Conclusion
Managing a patient with a nephrostomy requires a holistic, multidisciplinary approach. Nurses play a key role in monitoring, maintaining site hygiene, educating patients, and coordinating care. With support from dietitians and physiotherapists, patients can maintain quality of life and reduce the risk of complications.